The 3D printing of a living heart valve brings hope for young patients with a heart defect. Read on to learn more about this truly remarkable achievement in tissue engineering.
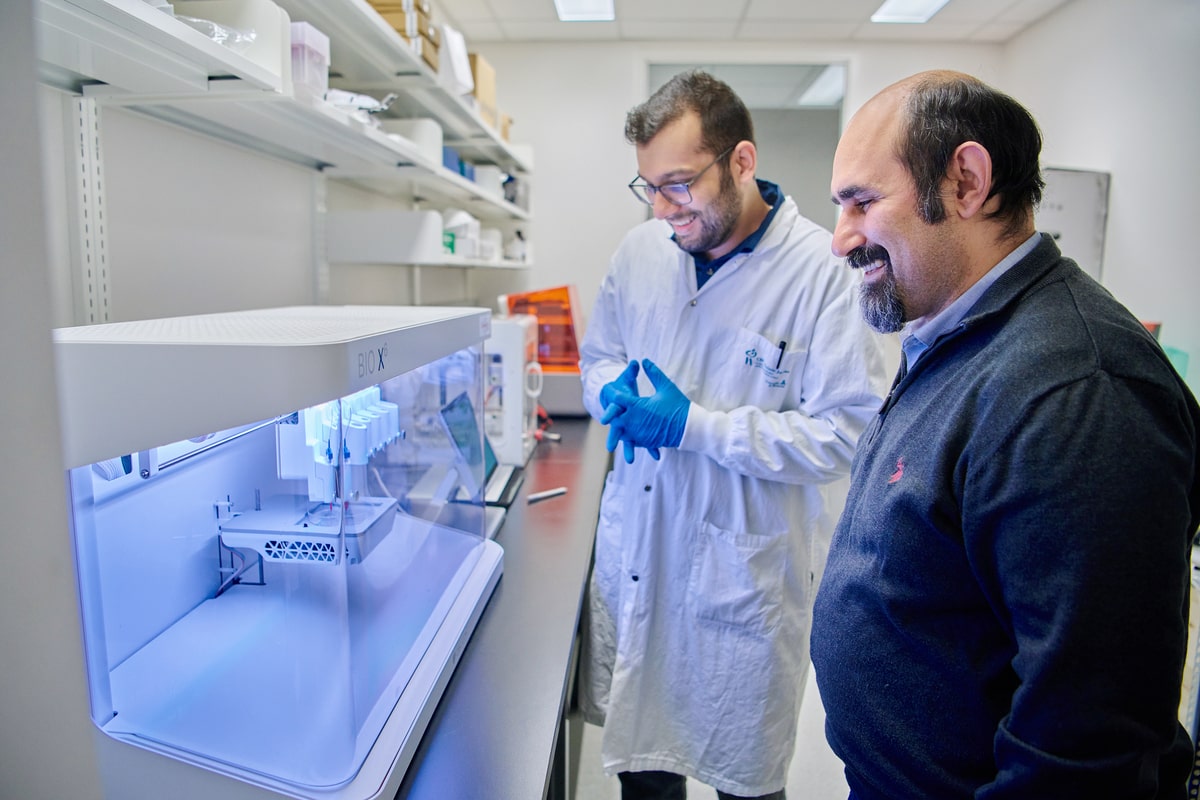
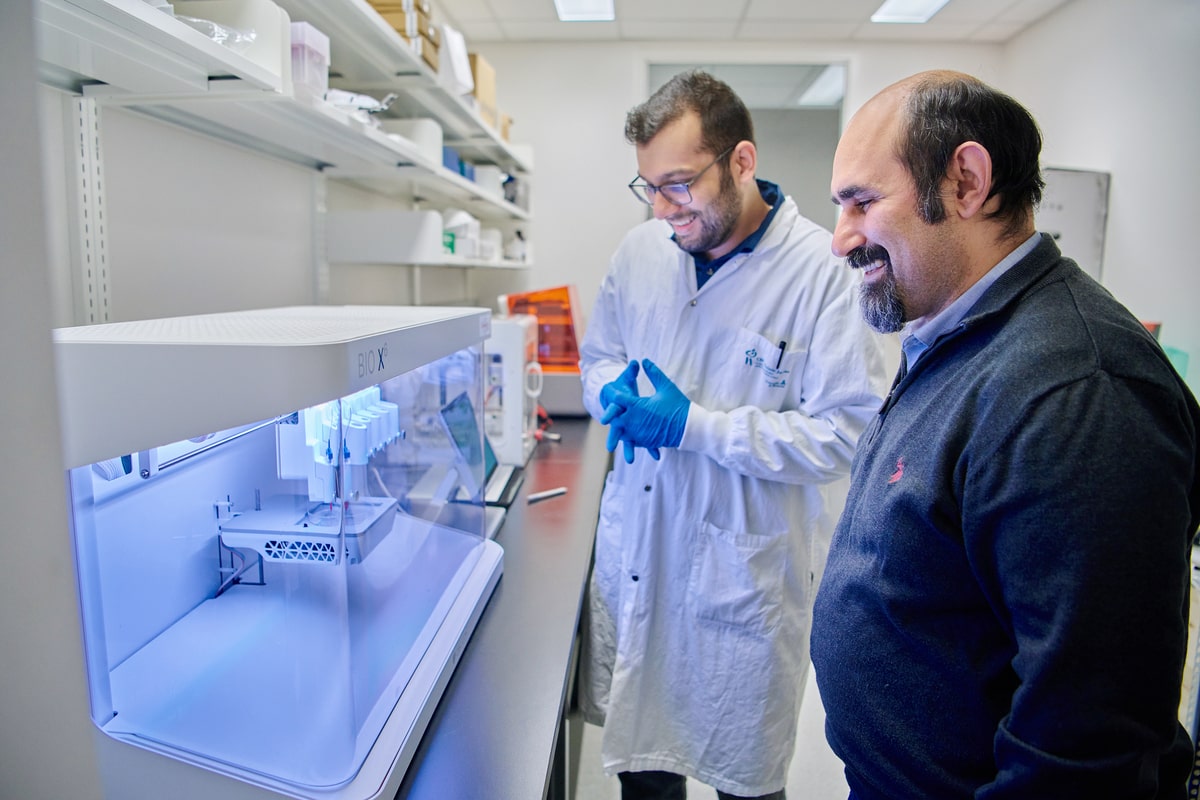
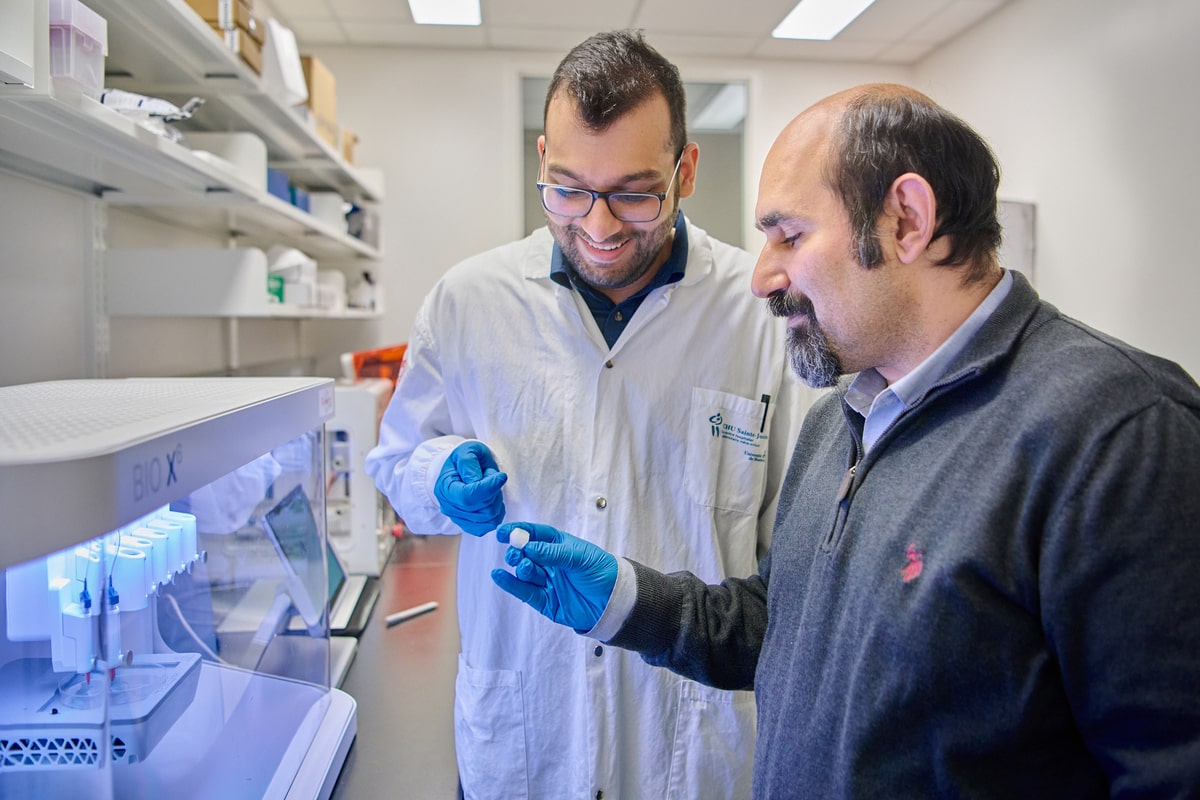
Imagine artificial heart valves that perform exactly like natural valves. At Sainte-Justine, real progress is being made toward that very goal. Earlier this year, research scientist Houman Savoji, PhD, and PhD candidate Arman Javari accomplished something extraordinary when they used 3D printing technology to produce a working heart valve.
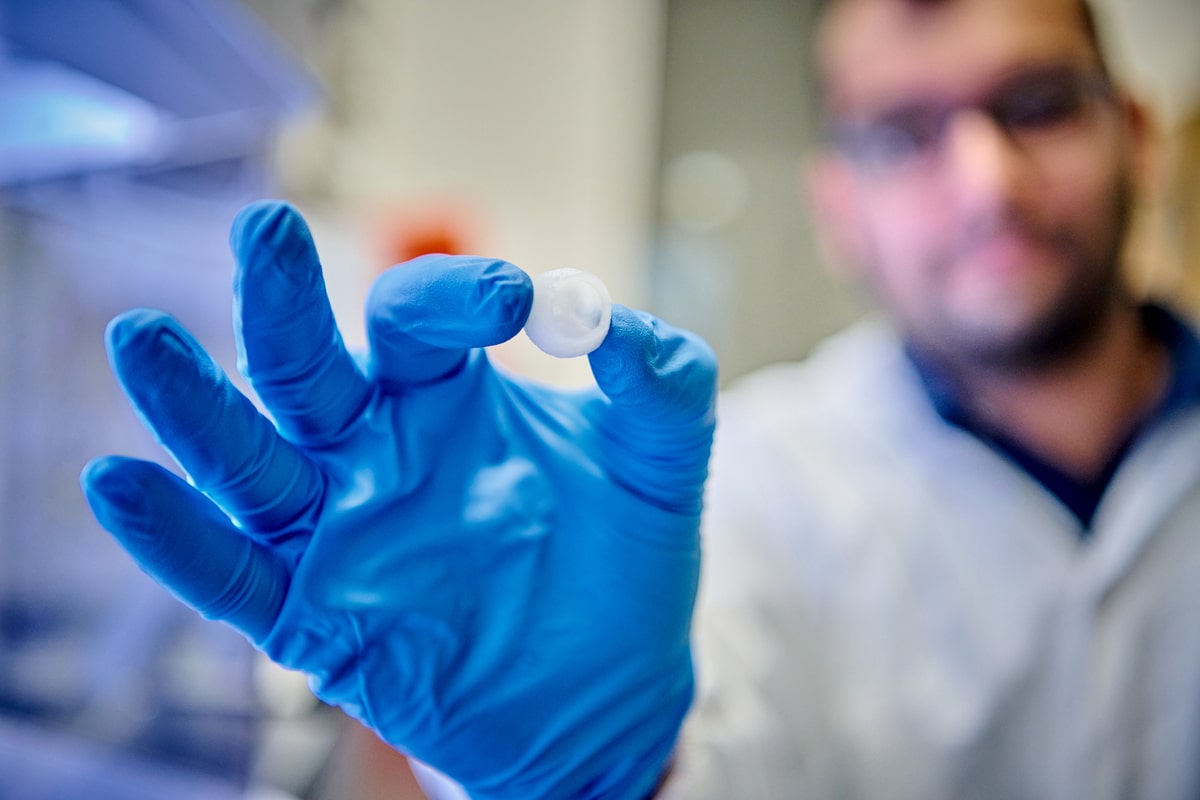
The result had the same texture as a real valve and behaved the same way. The findings of initial lab tests with mechanical pumps were very promising indeed. The movement of the artificial valve was identical to that of its natural counterpart. Nothing interfered with the flow of blood and there was no leaking when the valve closed. This bodes well for the ability of the printed valve to effectively channel blood to the circulatory system.
This breakthrough in tissue engineering has been greeted with tremendous enthusiasm. The characteristics of the new materials that have been developed have the properties scientists have been seeking: they are not rejected by the immune system; they have the potential of being able to integrate with other tissues; and they can be “seeded” with living cells that will then grow onto the printed surface.
Filling an enormous gap in pediatric medicine
According to Dr. Gregor Andelfinger, pediatric cardiologist and research scientist at Sainte-Justine, hundreds of children in Canada need a valve replacement every year, making this one of the most frequent pediatric operations.
Right now, young patients are given mechanical or biological valve transplants. Because these transplants are not made of living tissue, calcium deposits tend to build up over time and cracks begin to form, interfering with their performance. The result for patients is fatigue, shortness of breath and chest palpitations. The only alternative when this occurs is additional surgery to replace the faulty valve.
The situation becomes more complex when we consider that children and their hearts are still developing. In other words, it is only a matter of time until they outgrow their replacement valves. This can mean multiple operations until they reach adulthood.

“Heart defects have a significant impact on children’s and families’ quality of life. Fortunately, we now have the tools to surgically correct these defects, but it’s always going to be a stopgap measure. Families know that repeat surgeries will be required, which is a nerve-racking prospect. With living heart valves, the hope of a one-time fix is very real.”
The secret ingredient: A special kind of bioink
It looks like the heart valve made by Houman Savoji, research scientist, and Arman Jafari, the PhD student who works with him, might just overcome this problem. The properties of the new materials that have been developed are very promising, which means they will be able to test the potential of the new valves to grow with the heart.
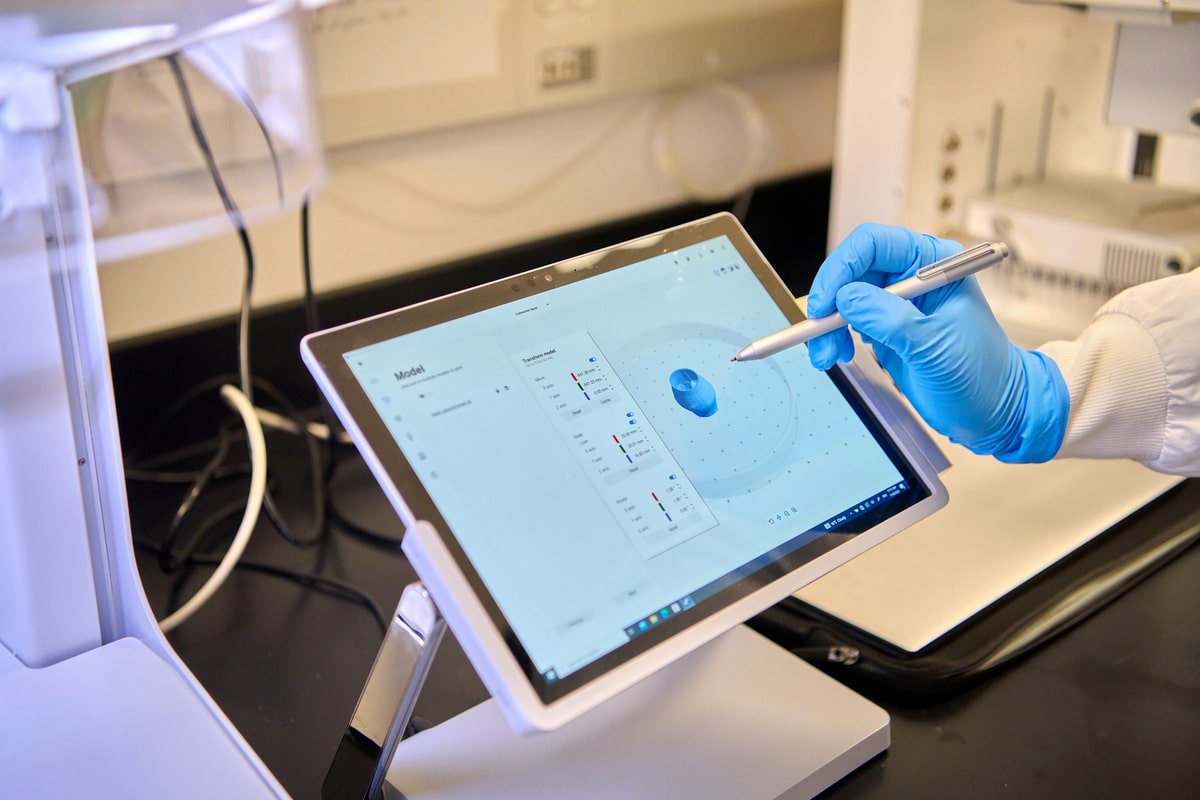
This fascinating achievement belongs to the realm of tissue engineering, a forward-looking discipline with a bright outlook. It combines the methodology and expertise of engineering and life sciences. The objective is to produce tissues or artificial organs using a patient’s own stem cells, which will have been directed toward a target destination in the lab. Tissue engineering techniques can be used to print structures (or “scaffolds”) with bioink, a special substance made of biomaterials and cells. The stem cells then attach themselves to the scaffold until the entire thing is replaced by living tissue. In other words, this technology taps into the patient’s own regenerating capacity to repair their own tissues.
Credits : Véronique Lavoie
“Heart valves printed with the special bioink that we have developed are biomimetic: they actually mimic the valves they will replace. They open and close like natural valves and function normally in an environment that reproduces human body conditions.”
Given that the cells used to produce the heart valve come from the patient, the risk of rejection is much lower than with other types of transplants.
Credits : Véronique Lavoie
From the research bench to patients’ bedsides
There are still plenty of steps to work through before the technology is available to young heart patients. To start, the findings have been published in a high-profile scientific journal. There will be several years of development and testing, similar to the process for a mechanical valve. The research team insists on passing all the tests required by international standards. So far, everything points to a positive outcome.
“The support we get from the community for our research makes all the difference. It gives us the freedom we need to make scientific breakthroughs like this living heart valve and use them to improve our patients’ lives.”
These kinds of ambitious projects are poised to transform the world of health care. They show just how much of an impact you are having on patient outcomes at Sainte-Justine. By empowering researchers to excel, you are giving them the tools they need to be at the forefront of scientific progress and fuelling hope for a healthier tomorrow for thousands of children and their families.